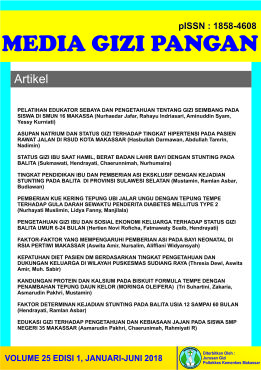
KERAGAMAN DAN PENERIMAAN MAKANAN ANAK BERPENGARUH PADA STUNTING DI DESA LOKUS STUNTING KABUPATEN ENREKANG : STUDI POTONG LINTANG
DOI:
https://doi.org/10.32382/mgp.v30i2.277Kata Kunci:
Keragaman, Penerimaan, Frekuensi Makan, StuntingAbstrak
Dietary Diversity Score (DDS), Acceptance Diet (AD) and Minimum Meal Frequency (FFM) of children's are direct variables that affect nutritional status. The objectives of this study was to determine the effect of DDS, FFM and AD on stunting in children aged 1-3 years. The Design is a cross-sectional study, conducted in Baraka District, Enrekang South Sulawesi Indonesia. Measurement of height using a microtoice (2-3) years and a length board (2 years) with an accuracy of 0.1 cm. Stunting was determined according to the 2006 WHO anthropometric median, <-2 SD HAZ. The child feeding instrument uses the WHO/Unicef instrument, 2021. Bivariate analysis used Chi Square Test, multivariate analysis used Logistics Regression. The results of the study found that the gender and father education had an effect on stunting (p=0.000) and p=0.018, while the age group (p=0.946), mother's occupation (p=0.392), mother's education (p=0.190) had no effect to prevention of stunting. Child feeding consisting of FFM, DDS and AD partially affected stunting p<0.05. Logistic regression analysis revealed that stunting can be predicted by modeling by 73.5% used strong predictors of risk factor DDS, and AD. Odds ratio 95% (CI) is 4.18 (1.69-10.33), p = 0.02 and 41.60(16.5-104.3) and protective by female Odds Ratio 95% CI= 0.30(0.12-0.71), p=0,007, Meanwhile, FFM and father education cannot predict stunting p=0.062 and p=0,442 respectively. Conclusion: stunting in Baraka sub-district is influenced by DDS, AD and Sex. It is recommended to strengthen education on the DDS and AD children to prevent stunting in children aged 1-3 years
Referensi
Abera, L., Dejene, T. and Laelago, T. (2018) ‘Magnitude of stunting and its determinants in children aged 6-59 months among rural residents of Damot Gale district; Southern Ethiopia’, BMC Research Notes, 11(1), pp. 1–6. Available at: https://doi.org/10.1186/s13104-018-3666-1.
Acharya, A., Pradhan, M.R. and Das, A.K. (2021b) ‘Determinants of minimum acceptable diet feeding among children aged 6-23 months in Odisha, India’, Public Health Nutrition, 24(12), pp. 3834–3844. Available at: https://doi.org/10.1017/S1368980021002172.
Aguayo, V.M. and Menon, P. (2016) ‘Stop stunting: Improving child feeding, women’s nutrition and household sanitation in South Asia’, Maternal and Child Nutrition, 12, pp. 3–11. Available at: https://doi.org/10.1111/mcn.12283.
Akombi, B.J. et al. (2017) ‘Stunting and severe stunting among children under-5 years in Nigeria: A multilevel analysis’, BMC Pediatrics, 17(1), pp. 1–16. Available at: https://doi.org/10.1186/s12887-016-0770-z.
Altmann, M. et al. (2018) ‘Effectiveness of a household water, sanitation and hygiene package on an outpatient program for severe acute malnutrition: A pragmatic cluster-randomized controlled trial in Chad’, American Journal of Tropical Medicine and Hygiene, 98(4), pp. 1005–1012. Available at: https://doi.org/10.4269/ajtmh.17-0699.
Aryastami, N.K. et al. (2017) ‘Low birth weight was the most dominant predictor associated with stunting among children aged 12–23 months in Indonesia’, BMC Nutrition, 3(1), pp. 1–6. Available at: https://doi.org/10.1186/s40795-017-0130-x.
Assefa, H., Belachew, T. and Negash, L. (2015) ‘Socio-demographic factors associated with underweight and stunting among adolescents in Ethiopia’, The Pan African medical journal, 20, p. 252. Available at: https://doi.org/10.11604/pamj.2015.20.252.3588.
Beal, T. et al. (2018) ‘A review of child stunting determinants in Indonesia’, Maternal and Child Nutrition, 14(4), pp. 1–10. Available at: https://doi.org/10.1111/mcn.12617.
Bommer, C., Vollmer, S. and Subramanian, S. V. (2019) ‘How socioeconomic status moderates the stunting-age relationship in low-income and middle-income countries’, BMJ Global Health, 4(1), pp. 1–10. Available at: https://doi.org/10.1136/bmjgh-2018-001175.
Cetthakrikul, N. et al. (2018) ‘Childhood stunting in Thailand: When prolonged breastfeeding interacts with household poverty’, BMC Pediatrics, 18(1), pp. 1–9. Available at: https://doi.org/10.1186/s12887-018-1375-5.
Dearden, K.A. et al. (2017) ‘Children with access to improved sanitation but not improved water are at lower risk of stunting compared to children without access: a cohort study in Ethiopia, India, Peru, and Vietnam’, BMC Public Health, 17(1), pp. 1–19. Available at: https://doi.org/10.1186/s12889-017-4033-1.
Dewey, K.G. (2016) ‘Reducing stunting by improving maternal, infant and young child nutrition in regions such as South Asia: Evidence, challenges and opportunities’, Maternal and Child Nutrition, 12, pp. 27–38. Available at: https://doi.org/10.1111/mcn.12282.
Dewey, K.G. et al. (2017) ‘Lipid-based nutrient supplementation in the first 1000 d improves child growth in Bangladesh: A cluster-randomized effectiveness trial’, American Journal of Clinical Nutrition, 105(4), pp. 944–957. Available at: https://doi.org/10.3945/ajcn.116.147942.
Faye, C.M., Fonn, S. and Levin, J. (2019) ‘Factors associated with recovery from stunting among under-five children in two Nairobi informal settlements’, PLoS ONE, 14(4), pp. 1–18. Available at: https://doi.org/10.1371/journal.pone.0215488.
Fink, G. et al. (2017) ‘Home- and community-based growth monitoring to reduce early life growth faltering: An open-label, cluster-randomized controlled trial’, American Journal of Clinical Nutrition, 106(4), pp. 1070–1077. Available at: https://doi.org/10.3945/ajcn.117.157545.
Galetti, V. et al. (2016) ‘Rural Beninese Children Are at Risk of Zinc Deficiency According to Stunting Prevalence and Plasma Zinc Concentration but Not Dietary Zinc Intakes’, The Journal of Nutrition, 146(1), pp. 114–123. Available at: https://doi.org/10.3945/jn.115.216606.
García Cruz, L.M. et al. (2017) ‘Factors associated with stunting among children aged 0 to 59 months from the central region of Mozambique’, Nutrients, 9(5), pp. 1–16. Available at: https://doi.org/10.3390/nu9050491.
Goudet, S. et al. (2015) ‘Nutritional interventions for preventing stunting in children ( 0 to 5 years ) living in urban slums in low and middle-income countries ( LMIC ) ( Protocol )’, Cochrane Database ofSystematic Reviews, (5), pp. 1–51. Available at: https://doi.org/10.1002/14651858.CD011695.www.cochranelibrary.com.
Guirindola, M.O. et al. (2018) ‘Determinants of meeting the minimum acceptable diet among filipino children aged 6-23 months’, Philippine Journal of Science, 147(1), pp. 75–89.
Halim, K. et al. (2020) ‘Associations of Dietary Diversity and Other Factors with Prevalence of Stunting among Children Aged 6-35 Months’, Indonesian Journal of Public Health Nutrition, 1(1), pp. 41–48. Available at: https://doi.org/10.7454/ijphn.v1i1.4380.
Hanson, S.K. et al. (2018) ‘Stunting at 24 months is not related to incidence of overweight through young adulthood in an urban South African birth cohort’, Journal of Nutrition, 148(6), pp. 967–973. Available at: https://doi.org/10.1093/jn/nxy061.
Huicho, L. et al. (2017) ‘Factors behind the success story of under-five stunting in Peru: A district ecological multilevel analysis’, BMC Pediatrics, 17(1), pp. 1–9. Available at: https://doi.org/10.1186/s12887-017-0790-3.
Hurley, K.M. et al. (2021) ‘A longitudinal impact evaluation of a comprehensive nutrition program for reducing stunting among children aged 6-23 months in rural Malawi’, American Journal of Clinical Nutrition, 114(1), pp. 248–256. Available at: https://doi.org/10.1093/ajcn/nqab010.
Kambale, R.M. et al. (2021) ‘Minimum acceptable diet among children aged 6–23 months in South Kivu, Democratic Republic of Congo: a community-based cross-sectional study’, BMC Pediatrics, 21(1), pp. 1–9. Available at: https://doi.org/10.1186/s12887-021-02713-0.
Kemenkes (2018) ‘Laporan Riskesdas Tahun 2018’.
Kemenkumham (2022) Peraturan Presiden Nomor 72 Tahun 2021 Tentang Percepatan Penurunan Stunting.
Khan, A.M. et al. (2012) ‘A study on infant and young child feeding practices among mothers attending an urban health center in East Delhi.’, Indian journal of public health, 56(4), pp. 301–304. Available at: https://doi.org/10.4103/0019-557X.106420.
Krishna, A. et al. (2018) ‘Trends in inequalities in child stunting in South Asia’, Maternal and Child Nutrition, 14(August 2017), pp. 1–12. Available at: https://doi.org/10.1111/mcn.12517.
Madinar (2021) ‘Fulfilment of minimum acceptable diet (MAD), short birth length and family income level are associated with stunting in children aged 6-23 months in Central Jakarta’, Malaysian Journal of Nutrition, 27(2), pp. 259–270. Available at: https://doi.org/10.31246/MJN-2020-0045.
Miller, A.C. et al. (2016) ‘How consistent are associations between stunting and child development? Evidence from a meta-analysis of associations between stunting and multidimensional child development in fifteen low- and middle-income countries’, Public Health Nutrition, 19(8), pp. 1339–1347. Available at: https://doi.org/10.1017/S136898001500227X.
Nahar, B. et al. (2012) ‘Effects of a community-based approach of food and psychosocial stimulation on growth and development of severely malnourished children in Bangladesh : a randomised trial’, 66(6), pp. 701–709. Available at: https://doi.org/10.1038/ejcn.2012.13.
Nkurunziza, S. et al. (2017) ‘Determinants of stunting and severe stunting among Burundian children aged 6-23 months: Evidence from a national cross-sectional household survey, 2014’, BMC Pediatrics, 17(1). Available at: https://doi.org/10.1186/s12887-017-0929-2.
Rahman, M.S. et al. (2016) ‘Association of low-birth weight with malnutrition in children under five years in Bangladesh: Do mother’s education, socio-economic status, and birth interval matter?’, PLoS ONE, 11(6). Available at: https://doi.org/10.1371/journal.pone.0157814.
Roba, K.T. et al. (2016) ‘Variations between post- and pre-harvest seasons in stunting, wasting, and infant and young child feeding (IYCF) practices among children 6-23 months of age in lowland and midland agro-ecological zones of rural Ethiopia’, Pan African Medical Journal, 24, pp. 1–9. Available at: https://doi.org/10.11604/pamj.2016.24.163.9387.
Roche, M.L. et al. (2017) ‘A Community-Based Positive Deviance/Hearth Infant and Young Child Nutrition Intervention in Ecuador Improved Diet and Reduced Underweight’, Journal of Nutrition Education and Behavior, 49(3), pp. 196-203.e1. Available at: https://doi.org/10.1016/j.jneb.2016.10.007.
Rolfe, E.D.L. et al. (2018) ‘Associations of stunting in early childhood with cardiometabolic risk factors in adulthood’, PLoS ONE, 13(4), pp. 1–14. Available at: https://doi.org/10.1371/journal.pone.0192196.
Ruel, M.T. and Alderman, H. (2013) ‘Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition?’, The Lancet, 382(9891), pp. 536–551. Available at: https://doi.org/10.1016/S0140-6736(13)60843-0.
Saaka, M., Wemakor, A., Abizari, A.-R., et al. (2015) ‘How well do WHO complementary feeding indicators relate to nutritional status of children aged 6–23 months in rural Northern Ghana?’, BMC Public Health, 15(1), p. 1157. Available at: https://doi.org/10.1186/s12889-015-2494-7.
Said-Mohamed, R. et al. (2015) ‘Has the prevalence of stunting in South African children changed in 40 years? A systematic review’, BMC Public Health, 15(1), pp. 1–10. Available at: https://doi.org/10.1186/s12889-015-1844-9.
Sanou, A.S. et al. (2018) ‘Association between stunting and neuro-psychological outcomes among children in Burkina Faso, West Africa’, Child and Adolescent Psychiatry and Mental Health, 12(1), pp. 1–10. Available at: https://doi.org/10.1186/s13034-018-0236-1.
Saxton, J. et al. (2016) ‘Handwashing, sanitation and family planning practices are the strongest underlying determinants of child stunting in rural indigenous communities of Jharkhand and Odisha, Eastern India: a cross-sectional study’, Maternal and Child Nutrition, 12(4), pp. 869–884. Available at: https://doi.org/10.1111/mcn.12323.
Sinha, B. et al. (2018) ‘Low-birthweight infants born to short-stature mothers are at additional risk of stunting and poor growth velocity: Evidence from secondary data analyses’, Maternal and Child Nutrition, 14(1), pp. 1–9. Available at: https://doi.org/10.1111/mcn.12504.
Sirajuddin, Saifuddin Sirajuddin, A Razak Thaha, Amran Razak, Ansariadi, R.M.T. (2020) ‘Evaluation Context And Mechanisms Of Stunting Intervention In Locus Area : A Systematic Review’, The 1st International Collaboration For Safety and Public Health, 31, pp. S828–S833. Available at: https://doi.org/10.1016/j.enfcli.2021.07.038.
van Stuijvenberg, M.E. et al. (2015) ‘Low intake of calcium and vitamin D, but not zinc, iron or vitamin A, is associated with stunting in 2- to 5-year-old children’, Nutrition, 31(6), pp. 841–846. Available at: https://doi.org/10.1016/j.nut.2014.12.011.
Takele, K., Zewotir, T. and Ndanguza, D. (2019) ‘Understanding correlates of child stunting in Ethiopia using generalized linear mixed models’, BMC Public Health, 19(1), pp. 1–8. Available at: https://doi.org/10.1186/s12889-019-6984-x.
Tassew, A.A. et al. (2019b) ‘Factors affecting feeding 6–23 months age children according to minimum acceptable diet in Ethiopia: A multilevel analysis of the Ethiopian Demographic Health Survey’, PLoS ONE, 14(2), pp. 1–14. Available at: https://doi.org/10.1371/journal.pone.0203098.
Thahir, A.I.A. et al. (2023) ‘Exploring Factors Associated with Stunting in 6-Month-Old Children: A Population-Based Cohort Study in Sulawesi, Indonesia’, Nutrients, 15(15), p. 3420. Available at: https://doi.org/10.3390/nu15153420.
Uwiringiyimana, V. et al. (2019) ‘Predictors of stunting with particular focus on complementary feeding practices: A cross-sectional study in the northern province of Rwanda’, Nutrition, 60, pp. 11–18. Available at: https://doi.org/10.1016/j.nut.2018.07.016.
Wagris, M. et al. (2019) ‘Minimum Meal Frequency Practice and Its Associated Factors among Children Aged 6 – 23 Months in Amibara District ’, Journal of Environmental and Public Health, 2019.
Wright, M.J. et al. (2015) ‘The interactive association of dietary diversity scores and breast-feeding status with weight and length in Filipino infants aged 6-24 months’, Public Health Nutrition, 18(10), pp. 1762–1773. Available at: https://doi.org/10.1017/S1368980015000427.
Zaragoza Cortes, J. et al. (2018) ‘Poor breastfeeding, complementary feeding and Dietary Diversity in children and their relationship with
Unduhan
Diterbitkan
Terbitan
Bagian
Lisensi
Hak Cipta (c) 2023 Sirajuddin, Agustian, Trina, Uti

Artikel ini berlisensi Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
PDF downloaded: 324